Illinois Collapsed Lung Injury Lawyers
5-Star Rated Attorneys for Victims of Pneumothorax from Car Accidents and Slip and Falls
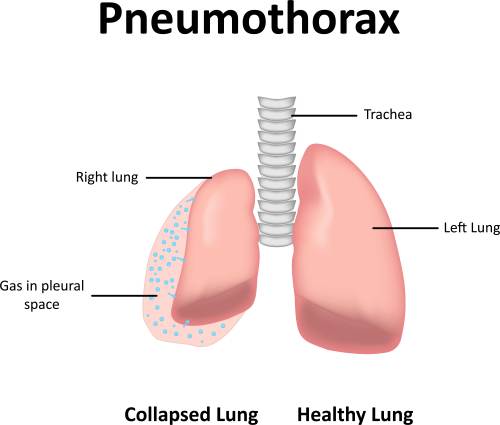
A collapsed lung, also known by the medical term pneumothorax, can be a frightening, painful, and dangerous event. It occurs when air accumulates in the space between the lung and the chest wall, causing all or part of the lung to collapse. At John J. Malm & Associates, we understand that a collapsed lung is not just a medical emergency; it’s a life-altering injury that can result from accidents, trauma, or medical negligence. Our Illinois personal injury attorneys have decades of experience helping Illinois residents recover from serious chest injuries, ensuring they receive the medical care, compensation, and support they need. Our team works tirelessly to investigate the circumstances of each case and advocate for those who have suffered from lung injuries due to someone else’s negligence.
What Is a Collapsed Lung?
Your lungs sit inside the chest (the thoracic cavity) inside a protective sac. Here’s how it works:
- The chest cavity has three compartments: two side compartments (the pleural cavities) that hold the lungs and a central compartment (the mediastinum) that holds the heart, major vessels, trachea, esophagus, and lymph nodes.
- Each lung is wrapped in a pleural sac, which consists of two continuous membranes:
- The visceral pleura: the layer that covers the lung itself.
- The parietal pleura: the layer that lines the inside of the chest wall, the diaphragm, and the mediastinum.
- Between those two membranes is the pleural cavity: the small space between the visceral and parietal pleura.
- Normally, this cavity has a tiny amount of fluid and negative pressure, which keeps the lung expanded. An analogy: imagine pushing your fist into an underinflated balloon. The balloon wall pushing around your fist is like the visceral pleura, the outer wall of the balloon is like the parietal pleura, and the space between them is the pleural cavity.
- A collapsed lung happens when air (or sometimes gas) accumulates in the pleural cavity. As more and more air builds up, it puts pressure on the lung so it cannot expand. The lung collapses partially or fully.
When the lung fully collapses, it is often referred to as a pneumothorax. If only part of the lung collapses or collapses due to loss of volume (instead of air entering the pleural space), that condition might be called atelectasis, which is different but related.
How Does a Collapsed Lung Occur?
There are many possible causes for a pneumothorax. The essential idea is that either the chest wall or the lung tissue is injured in a way that allows air to leak into the pleural space. Common causes include:
- Blunt-force injury or trauma to the chest: For example, from a fall, a motor vehicle accident, fractured ribs, or a crushing injury. A fractured rib can puncture the lung or let air track into the pleural space.
- Puncture wounds: A penetrating injury to the chest (such as from a knife or bullet) can allow air directly from the outside into the pleural cavity.
- Medical procedures: Some diagnostic or therapeutic procedures (biopsies, thoracentesis, mechanical ventilation) may inadvertently puncture the lung or pleura and cause air leakage.
- Underlying lung conditions: Diseases such as chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, pneumonia, emphysema, tuberculosis or lung cancer weaken lung tissue or cause blebs (small air blisters) that can rupture.
- Activities involving sharp changes in pressure: For example, deep‐sea diving, scuba diving, or flying at altitude may trigger a collapse in susceptible individuals because of pressure changes.
- Ventilator-related collapse: In patients on mechanical ventilation, positive-pressure breathing may contribute to alveolar rupture or barotrauma, leading to pneumothorax.
- Rupture of small air blisters (subpleural blebs): These sometimes develop at the top of the lungs, especially in tall, thin young men, and can spontaneously rupture, letting air escape into the pleural space for no obvious external trauma.
Sometimes, a pneumothorax occurs spontaneously, that is, without obvious trauma or medical procedure. The cause may not be immediately identifiable.
Types of Personal Injury Claims That May Involve Collapsed Lungs
Collapsed lungs often result from serious accidents or injuries. Common personal injury claims where pneumothorax may occur include:
- Motor vehicle accidents: Airbags, seatbelt trauma, steering wheel impact, or collisions that fracture ribs or puncture the chest.
- Slip and fall accidents: Falls from height or on icy surfaces, causing blunt chest trauma.
- Workplace accidents: Construction site falls, heavy object strikes, or equipment accidents leading to chest injuries.
- Medical malpractice: Injuries caused during procedures such as lung biopsies, catheter insertions, or improper ventilator use.
In any of these cases, a collapsed lung can lead to hospitalization, long-term medical care, and life disruption, which is why proper documentation and medical treatment are critical.
Statistics on Pneumothorax Injuries
While national statistics give us a baseline of incidence, it helps to understand your risk and the significance of a pneumothorax in Illinois.
Risk and incidence:
- In general U.S. data, the annual incidence of primary spontaneous pneumothorax (PSP) in adults is estimated at about 7.4 to 18 cases per 100,000 men and 1.2 to 6 cases per 100,000 women.
- Secondary spontaneous pneumothorax (SSP) (due to underlying lung disease) is around 6.3 per 100,000 men and 2.0 per 100,000 women annually.
- If you have lung disease, a history of smoking, or trauma in Illinois, your risk of a lung collapse is higher than average.
Why it matters for Illinois drivers/accident victims:
- In an accident scenario (motor vehicle collision, fall, etc.), a chest trauma causing a pneumothorax may significantly increase medical costs, length of hospital stay, and potential compensation in a personal injury context.
- Understanding that pneumothorax is a recognized medical condition with serious consequences is important for recovery planning, treatment, and legal or insurance discussions.
What Are the Symptoms of a Collapsed Lung?
Symptoms of a pneumothorax depend on how much of the lung is collapsed, how quickly it occurred, and whether underlying lung disease is present. Some people with very small collapses may have minimal or no symptoms; others with a large or sudden collapse can experience dramatic effects.
Typical symptoms include:
- Sudden onset of sharp or stabbing chest pain (often on one side, can radiate to the shoulder) made worse by deep breaths or coughing
- Sudden shortness of breath (dyspnea)
- Rapid breathing (tachypnea)
- Rapid heartbeat (tachycardia)
- Chest tightness
- Skin turning bluish (cyanosis) in severe cases due to lack of oxygen
- Feeling lightheaded or faint
- General fatigue or weakness
If a collapse is minor, symptoms may be mild or even absent. But if you start experiencing sudden chest pain and breathlessness, especially after trauma or due to lung disease, this should be evaluated immediately.
How is a Collapsed Lung Diagnosed?
If your medical team suspects a pneumothorax, several steps are commonly taken:
- Physical examination
- The doctor listens to your lungs. In a collapsed lung, breath sounds may be reduced or absent on the affected side.
- Other signs may include hyper‐resonance to percussion, decreased tactile fremitus, or distended neck veins in severe cases.
- Imaging tests
- Chest X-ray: The main initial tool. It can show a visible pleural line without lung markings beyond it (indicating air in the pleural space).
- CT scan (Computed Tomography): Provides more detailed imaging and may be used if other injuries are suspected, or the cause is unclear.
- Ultrasound: Increasingly used, especially at the bedside, to detect even small amounts of pleural air in real time.
- Blood tests (Arterial Blood Gas – ABG)
- Measures oxygen and carbon dioxide levels in the blood. A collapse of the lung may lead to lower oxygen and higher carbon dioxide. This helps assess how much the lung function is impaired.
The diagnostic process aims to determine the size of the collapse, any underlying lung disease, the cause (trauma, spontaneous, procedure‐related), and plan the optimal treatment.
Treatment of a Collapsed Lung
The goal of treatment is twofold: relieve the pressure on the lung so it can expand again and prevent a recurrence (if possible). The method chosen depends on the patient’s symptoms, size of the collapse, cause, and overall lung health.
Treatment options include:
- Observation (“watch and wait”) + high flow oxygen:
- For very small pneumothoraces in stable patients (especially primary spontaneous ones) who are minimally symptomatic: sometimes simply observing, administering supplemental oxygen and monitoring is sufficient. Oxygen can help speed up the absorption of the air in the pleural cavity.
- Needle aspiration:
- For moderate collapses in stable patients, a small needle or catheter may be used to draw the air out of the pleural space. This approach has been shown to succeed in ~70% of selected patients.
- Chest tube (thoracostomy) insertion:
- For larger or symptomatic pneumothoraces, traumatic causes, or patients with underlying lung disease: placing a larger tube to evacuate air and allow lung re-expansion is standard.
- Surgery or pleurodesis:
- If the air leak persists (typically more than 3-5 days) or there are recurrent episodes, more advanced interventions are considered, such as chemical pleurodesis (talc, doxycycline), video‐assisted thoracoscopic surgery (VATS) to remove blebs and attach the lung to the chest wall, etc.
Factors in choosing treatment:
- Size of collapse (often measured by radiograph rim > 2 cm indicates larger collapse).
- Symptoms: breathlessness, chest pain, hemodynamic instability.
- Underlying lung disease: patients with COPD, severe asthma, etc., tend to require more aggressive treatment (secondary spontaneous pneumothorax).
- Cause: traumatic or iatrogenic (after a procedure) pneumothorax tends to be treated more aggressively.
- Recurrence risk: If this is your second (or more) collapse, surgery or pleurodesis may be considered.
- Other considerations: e.g., aviation or diving plans (since residual or unresolved pneumothorax is a contraindication to flying or diving).
Recovery and monitoring:
- Once treated, monitoring with chest X-rays or ultrasound is needed to confirm full re-expansion of the lung and that no new air leak is present.
- Patients are often advised to avoid air travel or scuba diving until full resolution is confirmed.
- Smoking cessation is crucial because smoking increases the risk of spontaneous pneumothorax significantly.
$125,000 Settlement. John J. Malm & Associates obtained a policy-limits settlement for a client who suffered a pneumothorax in a multi-vehicle car accident.
$100,000 Settlement. John J. Malm & Associates obtained a policy-limits settlement of $100,000 for a client injured in a single vehicle accident, wherein she suffered a collapsed lung, requiring extensive emergency treatment.
Why Pneumothorax Matters After an Accident
If you or a loved one has experienced chest trauma (from a car crash, fall, or other accident) or has underlying lung disease and develops a collapsed lung, understanding this condition is essential for recovery.
- A collapsed lung can be life-threatening if not treated, especially if it becomes a tension pneumothorax (where pressure builds dangerously in the pleural space).
- The severity of injury, need for longer hospital stay, risk of recurrence, and long-term impacts (such as limitations on air travel or returning to certain activities) mean it can shape your life for months or years.
- If trauma was involved (for example, a car accident in Illinois) and you suffer a pneumothorax, documenting the cause and obtaining appropriate treatment is critical.
- Recovery may require chest tube placement, surgery, or careful monitoring and delays or mismanagement can increase complications.
Frequently Asked Questions about Collapsed Lungs
Q: Can a small collapse of the lung heal on its own?
A: Yes, in selected cases of very small pneumothoraces (especially primary spontaneous ones in healthy individuals with minimal symptoms), observation + oxygen may suffice. However, this must be done under medical supervision with regular follow-up.
Q: What is a tension pneumothorax and how is it different?
A: A tension pneumothorax is a severe form where air continues to leak into the pleural space and cannot escape, building pressure that compresses the lung and mediastinal structures (heart, vessels). It is a medical emergency. Signs include low blood pressure, neck vein distension, and tracheal shift in severe cases. Immediate decompression is required.
Q: After I have a collapsed lung, when can I fly or go scuba diving?
A: Because changes in pressure can enlarge or trigger a pneumothorax, patients are advised to avoid air travel or diving until full resolution is confirmed by imaging. Some guidelines say to wait at least 7 days after a documented full resolution.
Q: Is smoking really that big a risk?
A: Yes. Smoking substantially increases the risk of a spontaneous pneumothorax. Some studies report smokers are up to 20-fold more likely than non-smokers.
Q: If I’ve had one collapsed lung, what’s the chance it will happen again?
A: Recurrence rates for primary spontaneous pneumothorax may reach 21-54% within 2 years.
Q: What symptoms warrant immediate emergency care?
A: Sudden chest pain and breathlessness, especially after trauma; low blood pressure; rapid heart rate; blue skin; difficulty breathing; any sign of shock or collapse. These signs call for 911 or a visit to the emergency department.
Q: What happens if a collapsed lung is missed or untreated?
A: Without treatment, it can enlarge, lead to complete lung collapse, hypoxia (low oxygen), or worsen into tension pneumothorax. That can risk heart and lung failure or even death in severe cases.
Contact the Top-Rated Illinois Pneumothorax Injury Lawyers at John J. Malm & Associates
A collapsed lung is a serious medical condition, but one that is often treatable, especially when caught early and managed properly. If you experienced chest trauma in an accident, or you suffer from lung disease and find yourself with sudden chest pain or breathlessness, don’t wait. Prompt diagnosis and treatment can make all the difference.
At John J. Malm & Associates, we help Illinois residents who have experienced serious chest injuries like pneumothorax navigate the recovery process and secure the compensation they deserve. Don’t face the medical, financial, and emotional challenges alone. Contact us today for a free consultation and let us help protect your health, your rights, and your future.